CASE STUDIES
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
AI-Powered Medication Safety: Turning Smarter Alerts into Safer Care
Medication errors cause tens of thousands of deaths annually in the U.S. Existing alert systems produce too many false positives, leading to clinician fatigue and ignored warnings. The client developed an AI-driven platform that sharply improved accuracy but needed a business case and integration strategy? to navigate complex healthcare incentives and prove value to hospitals and payers.
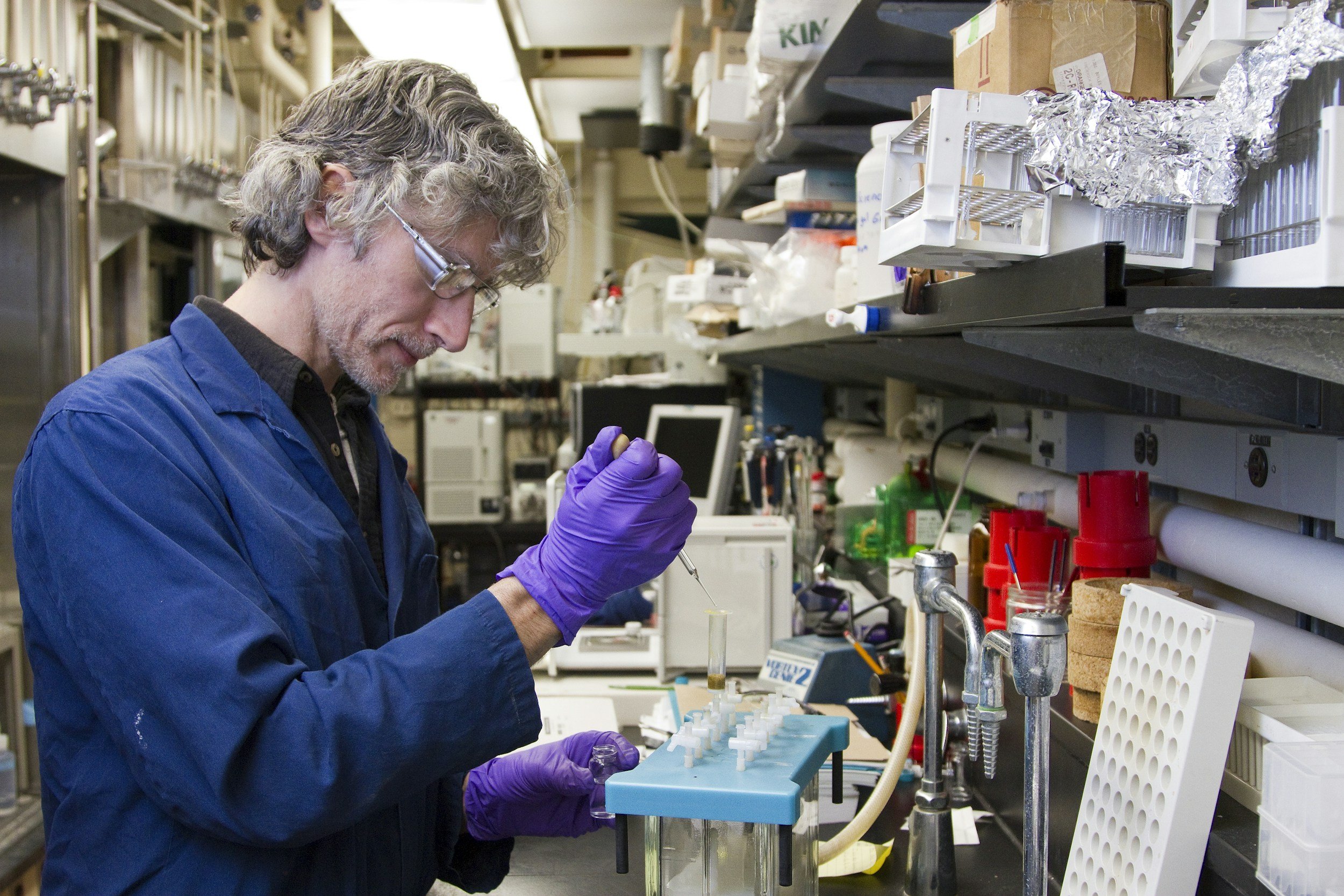
AI-Powered Liquid Biopsy: From Bench to Bedside
The client sought to replace traditional invasive biopsies with a noninvasive, AI-driven imaging and analytics platform capable of real-time cancer detection. The technology showed strong promise across multiple cancers but faced a crowded diagnostics landscape, complex regulatory pathways, and questions about market entry strategy and investor appeal.
Strategic AI Assessment: Positioning a Healthcare Data Leader for the Next Wave
AI is reshaping healthcare data, decision support, and drug discovery. The client was a dominant player in clinical decision support and ePrescribing but faced rising competition from AI-driven startups entering adjacent spaces. Leadership needed a clear picture of where AI posed threats, where it opened opportunity, and how to realign strategy for sustainable growth.
AI Platform Strategy: From Open-Source Experiment to Ecosystem Engine
The client built an open-source marketplace connecting healthcare developers, researchers, and organizations to share and deploy data-driven applications. With hundreds of contributors and growing traction among developers, the company needed to convert community enthusiasm into enterprise demand among health systems, life-sciences firms, and payers. Leadership sought a scale-up strategy to attract institutional users and prepare for Series A fundraising.
Pivoting to Clinical Trials: Turning Pandemic Experience into a Growth Engine
When COVID-19 shut down workplaces, the client’s mobile vision-testing business evaporated overnight. They successfully repurposed their mobile centers to support pharmaceutical trials but were uncertain whether to build a long-term clinical-trials business once normal operations resumed.
Interoperability as Opportunity: Repositioning for Accelerated Growth
New interoperability rules threatened to erode demand for the client’s core hospital indexing product. Leadership needed to gauge how much risk the regulation posed and to identify growth paths beyond hospitals.
Retail Embraces Digital Health: Creating an Integrated Consumer Platform
The client planned to build in-store health clinics but lacked a digital bridge to unify customer health engagement. The innovation group sought guidance on how to design and prioritize digital offerings that complemented its physical assets.
Consumer-Pay RPM: Expanding Beyond the Physician Channel
The client’s physician-office sales model constrained growth. They wanted to test whether a direct-to-consumer offering could accelerate adoption and feed physician demand.
Strengthening Hospital Cybersecurity: From Crisis Response to Collective Resilience
Ransomware attacks had driven up insurance premiums and threatened coverage for member hospitals. The association needed a plan to protect members and restore insurer confidence.
Molecular Diagnostics: Making the Right Technology Choice
A breakthrough technology promised faster, simpler disease-activity testing but clashed with the firm’s original complex platform. Board, founder, and management were deadlocked over which path to pursue.
CDMO Due Diligence: Pinpointing Opportunity in a Complex Market
The investor signed a letter of intent to acquire a fast-growing contract development and manufacturing organization (CDMO) but lacked sector experience. They needed to validate market attractiveness, customer stickiness, and management strength before closing.
CCM/RPM Diligence: Testing Investment Thesis Under Regulatory Uncertainty
A potential acquisition in chronic care management and remote monitoring showed promise but came with reimbursement and policy risk. The investor needed clarity on sustainability and growth levers before bidding.
Temperature-Controlled Packaging: Positioning for a Successful Exit
Evolving environmental standards and pandemic-driven vaccine transport created volatility in the temperature-controlled packaging market. The company needed an independent market study to educate buyers and strengthen its sale narrative.
Temperature-Controlled Packaging: From Diligence Insight to Market Expansion Strategy
When a private-equity investor considered acquiring an innovative supplier of reusable temperature-controlled packaging (TCP), they turned to HBG for commercial diligence. The deal team needed to validate market growth, competitive positioning, and regulatory and pharmaceutical-industry risks before proceeding.
Temperature controlled packaging
A leading, private equity sponsored temperature controlled packaging company sought assistance in positioning itself for sale. Client engaged HBG to conduct a market study and to present findings to leading bidders.
Decentralized clinical trials
A company that provided mobile vision centers for office workers switched to supporting clinical trials during the pandemic. With normalcy returning, the company needed help to decide whether to invest in building a clinical trials business for the long term.
Medical record interoperability
Client was a leader in electronic medical record indexing, working with major hospital systems to ensure continuity of care. With the implementation of new interoperability rules, it was imperative for the company to develop strategic growth options in adjacent markets. Client required consulting support to provide expertise outside of the hospital segment.
Digital health for leading retailer
A leading retailer had decided to enter the healthcare space, with a focus on in-person clinics and other physical assets. The Client’s innovation group sought support to develop and prioritize complementary digital offerings.
Remote Patient Monitoring
A remote patient monitoring (RPM) company that marketed to physician offices wanted to accelerate its growth by adding a consumer pay offering. Health Business Group conducted consumer market research, identified partnership opportunities, and developed a go to market plan.
Hospital Cybersecurity
Following a wave of cyberattacks, hospitals struggled to retain cyberinsurance coverage and prevent premiums from skyrocketing. They turned to their state hospital association for help. Health Business Group leveraged expertise in cybersecurity and healthcare to recommend a course of action.